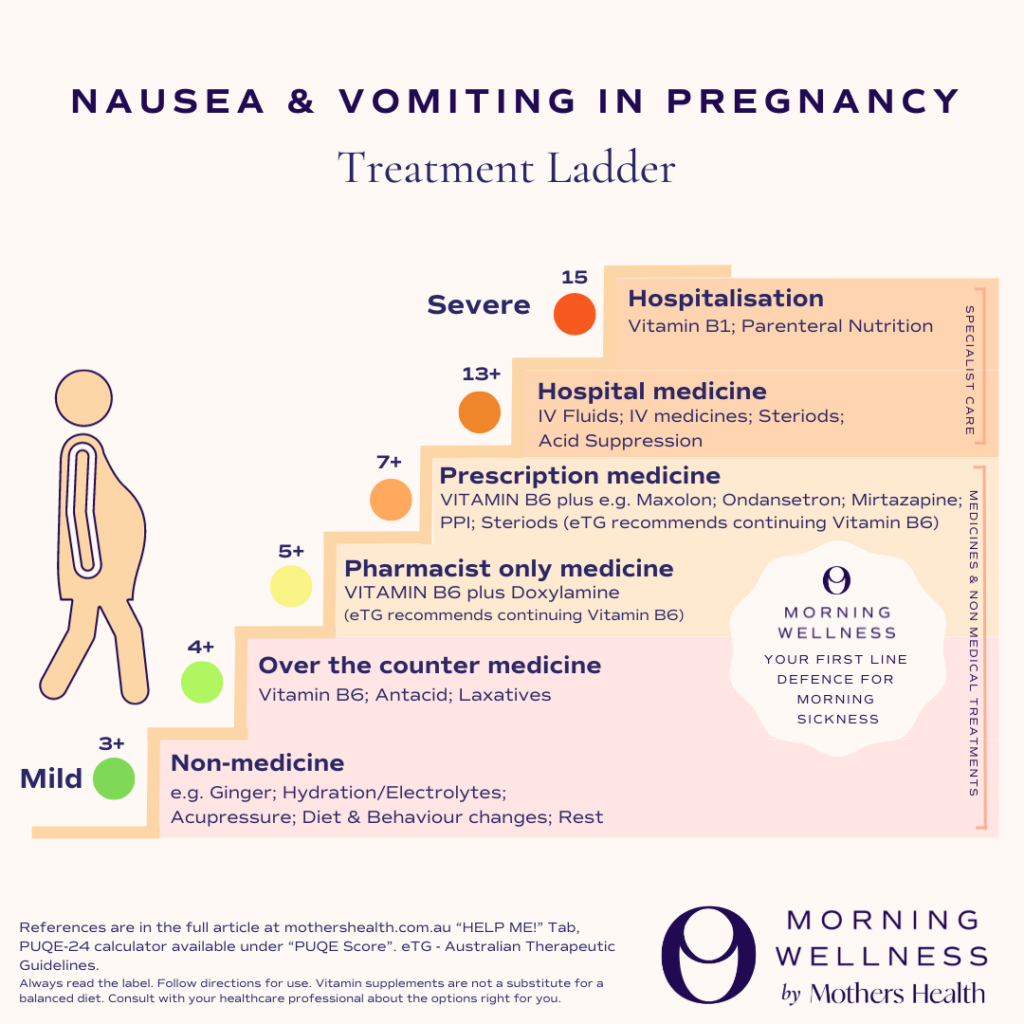
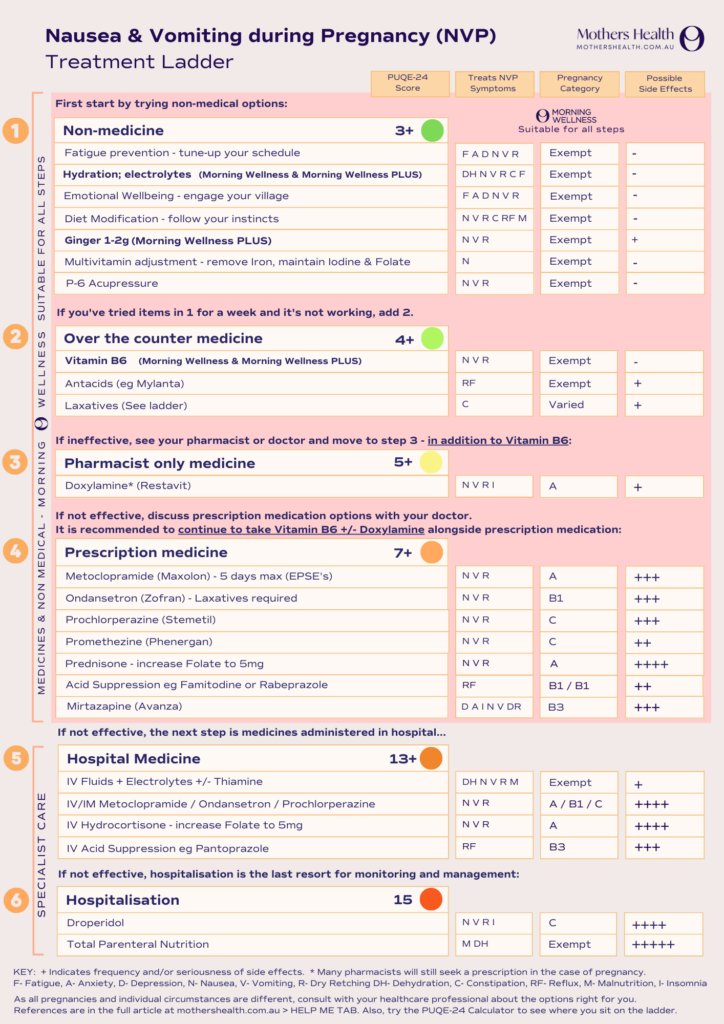
Nausea and Vomiting during Pregnancy Treatment Ladder
Article and NVP ladder written by Dr Roly Stokes
Images developed by AMber McDonald
You’re pregnant!! Great!!
Or is it?
Morning Sickness can really suck the fun out of pregnancy (and worse). The thing is, you don’t have to put up with it – there are solid options available to get you back to the famous pregnancy glow.
More appropriately known to doctors as Nausea and Vomiting during Pregnancy (NVP), morning sickness does not happen only in the morning. In fact, it is an extremely variable issue, ranging from zero symptoms in those lucky few; to moderate symptoms for the many; and in rare cases, it can be extreme enough to require hospital admission. The good news is that almost never does the baby feel any impact – even if you draw the short straw and land on the most severe end of the NVP spectrum – Hyperemesis Gravidarum (HG).
NVP usually starts around week 6 of gestation – week 4 after conception. For half of affected women, it settles down around week 14, with 90% of mamas finding relief by week 22. For every mum, it completely resolves after delivery. Importantly, if you develop new nausea and vomiting (especially after week 9), you need to be cautious that the symptoms are not from something else – a kidney infection is a relatively common copycat – so if you’re at all unsure, please see your GP pronto.
To help women get the important care they need, doctors have developed a scoring system to assess the severity of NVP, creatively named the ‘PUQE-24’ score. It stands for ‘Pregnancy Unique Quantification of Emesis’ which assesses NVP severity over 24 hours. The PUQE has been shown to closely reflect women’s self-reported estimates of suffering, as well as objective things like rates of hospitalisations. It’s great to have a really solid score like this to track your illness because sometimes doctors may underestimate severity, or it might help you understand when it’s time to climb the ladder and get more help. Calculate your PUQE-24 score here.
When we talk about NVP, or morning sickness, it’s easy to assume that the only symptoms are nausea, vomiting and dry retching, however – as if these weren’t bad enough – there is a ‘secret’ second wave of symptoms. Unfortunately dehydration, reflux, constipation, fatigue, and emotional struggles are all very real, direct consequences of NVP. Rarely, NVP can also lead to malnutrition and – in the most extreme cases only – adverse pregnancy outcomes.
Fortunately each of these symptoms can be treated – and the sooner and more effectively they are treated, the better off you and your bub will be.
To make things easier, and to clear some of the information swamp, we have trawled through the leading guidelines (8,9,10) and developed a simple stepwise approach to the treatment of NVP.
Welcome to the Mothers Health Nausea and Vomiting during Pregnancy Treatment Ladder.
Non-medicine therapies
PUQE Score 3+
If you talk to a mother who has had NVP before you’ll hear a myriad of old wives treatments, traditional recipes and NVP hacks that they swear by. The truth is that (mostly) they are worth trying because they’re typically free or cheap and very low risk – and they might just work for you and your NVP! If you get suggestions of therapies that cost an arm and a leg, or sound risky, then it might be smarter to pass and work your way up the ladder instead.
In order of importance:
1. Sleep
Treats: Fatigue, Anxiety, Depression, Nausea, Vomiting, Dry Retching.
Sleep and rest are when we have a chance to recover, reset and rebuild – and these are all especially important in pregnancy. It has been shown that inadequate sleep exacerbates the symptoms of NVP, so ensuring a good night’s sleep is paramount – and it is something we have (some) control over.
- Set aside an uninterrupted 8 hour window at night
- Completely black out your windows
- Ditch the screens at least an hour before bed
- Tape over any LEDs/lights in your bedroom
- Develop a set night time routine
- Allow a steady temperature drop over the night (avoid A/C)
- Take naps!
And a hack for when your bubba arrives – most of these sleep hygiene tips work for kiddos older than 3 months, though they do need more hours of sleep than adults.
2. Hydration
Treats: Dehydration, Nausea, Vomiting, Dry Retching, Constipation, Fatigue
Hydration is critical for us to function as humans. You can survive weeks or months without food, but you can survive only days without water and your baby is no different. The challenge to stay hydrated is increased in NVP as nausea can make it hard to tolerate anything by mouth PLUS vomiting itself actually depletes electrolytes. The struggle is real, but paying attention to these tips might be the difference between needing a trip to hospital for IV fluids or not. If you ever feel dizzy, or lightheaded it might suggest you’re short on hydration.
- Aim for at least 2L a day of water
- ‘The Home Drip’ – Sip 5-30mL every 5mins for at least an hour, then increase volume as you gain strength
- Suck on ice chips or ice blocks
- Try cold drinks
- Avoid caffeine
- Try warm or hot water
- Drink through a straw or use a sippy cup to avoid drink smells triggering symptoms
- Regular Electrolytes – especially important if vomiting or not eating any food
- Daily weight measurement – 5% weight loss from pre-pregnancy weight is a red flag and you need to get to the doc pronto.
3. Emotional Wellbeing
Treats: Fatigue, Anxiety, Depression, Nausea, Vomiting, Dry Retching
This is huge. Women with NVP are more at risk of more severe mental health challenges. Simply put, the more severe the vomiting, the greater impact upon quality of life, and the more significant the risk of depression.
You know the village they talk about? That starts now. The presence of at least three support people has been shown to be protective against depression and even reduce NVP itself, so engage your village.
Your health care professional is a significant part of your care here. If they don’t take your symptoms seriously and they don’t get you started on treatments asap, you seriously need to move on to someone who does. Your emotional and physical health depends on it.
If you need help right now, try these:
Australia
https://panda.org.au/get-support/support-expecting-a-baby
https://www.gidgetfoundation.org.au/
https://www.beyondblue.org.au/
NZ
https://pada.nz/depression-and-anxiety-in-pregnancy/
https://healthify.nz/health-a-z/d/depression-perinatal/
4. Diet Modification
Treats: Nausea, Vomiting, Dry Retching, Constipation, Reflux, Malnutrition
Anything that enters your stomach has the capacity to trigger queasiness. Careful management about what goes in can help substantially. Unlike hydration, and unless you have certain medical conditions, it’s not a disaster if you can’t get anything down at meal times. If you’re unable to get anything down at all for 24 hours, it’s probably time to go up the ladder. If not, try these tips:
- Avoid strong smells
- Avoid spicy food
- Eat smaller meals more often
- Follow your cravings – if you can only eat nuggets and it happens to be breakfast, then have nuggets for breakfast!
- Higher carb, lower fat meals
- Try high protein snacks
- Crackers or plain biscuits are a common winner
- Change your multivitamin to one that does not contain iron. Caution with this one: if you are anaemic, low iron or unsure of your haemoglobin please discuss with your doctor.
- High fibre food will help with any constipation; try fruit & veg – bananas or kiwifruits are a great place to start.
5. Acupressure
Treats: Nausea, Vomiting, Dry Retching
Acupressure originated in ancient China. It is based on the fundamental principle of acupoint activation across the meridians, and is typically performed by applying thumb or hand pressure on specific acupoints in the body. For NVP, the most common acupoint is the P6, which lies between two tendons in the forearm, four centimetres from the wrist crease. Studies are hard to compare for NVP as they are dissimilar in the nature of the patients and contexts.
There are circumstances when P6 acupressure seems to be effective for NVP and circumstances where it may not, however given its relatively low risk of negative outcomes, it is something that could be considered.
If the non-medicine options haven’t helped after one week then it is time to start climbing the NVP treatment ladder and to try medicine.
Medicines
When we think ‘sickness’, we think ‘medicine’. Medicines are a preparation given to treat or prevent a disease and they’re popular for good reason! Medicines are easy to take and have been studied closely to maximise effectiveness whilst minimising side effects.
The thing is, medicines vary in effectiveness and side effects. The unicorn medicine is 100% effective, with 0% side effects, however, just as with life partners, there is no unicorn medicine and each medicine has a pros and cons list.
The Australian medicine system is arranged in such a way to minimise the risk of harm from nasty side effects. It does this by regulating the availability of medicines through a tiered system:
- Food as medicine / Natural medicine – can be sold anywhere (generally low risk) eg Ginger
- Over the counter medicine – can be sold anywhere (low risk) E.g. Vitamin B6, paracetamol
- Pharmacy only medicine – can only be sold by a pharmacist (medium risk) E.g. doxylamine
- Prescription only medicine – can only be sold by a pharmacy with a prescription from a doctor (higher risk) – E.g. ondansetron
- Authority only medicine – can only be sold by a pharmacy with a prescription from a doctor with special authority (high risk) E.g. morphine
The important point here is that this hierarchy is linked to safety NOT effectiveness. Just because you can buy paracetamol from a servo doesn’t mean it’s an inferior painkiller to morphine, it just means it is a much safer painkiller than morphine. Actually paracetamol is a very effective painkiller and we’re very lucky that it has a very low side effect profile so we can buy it from the servo!
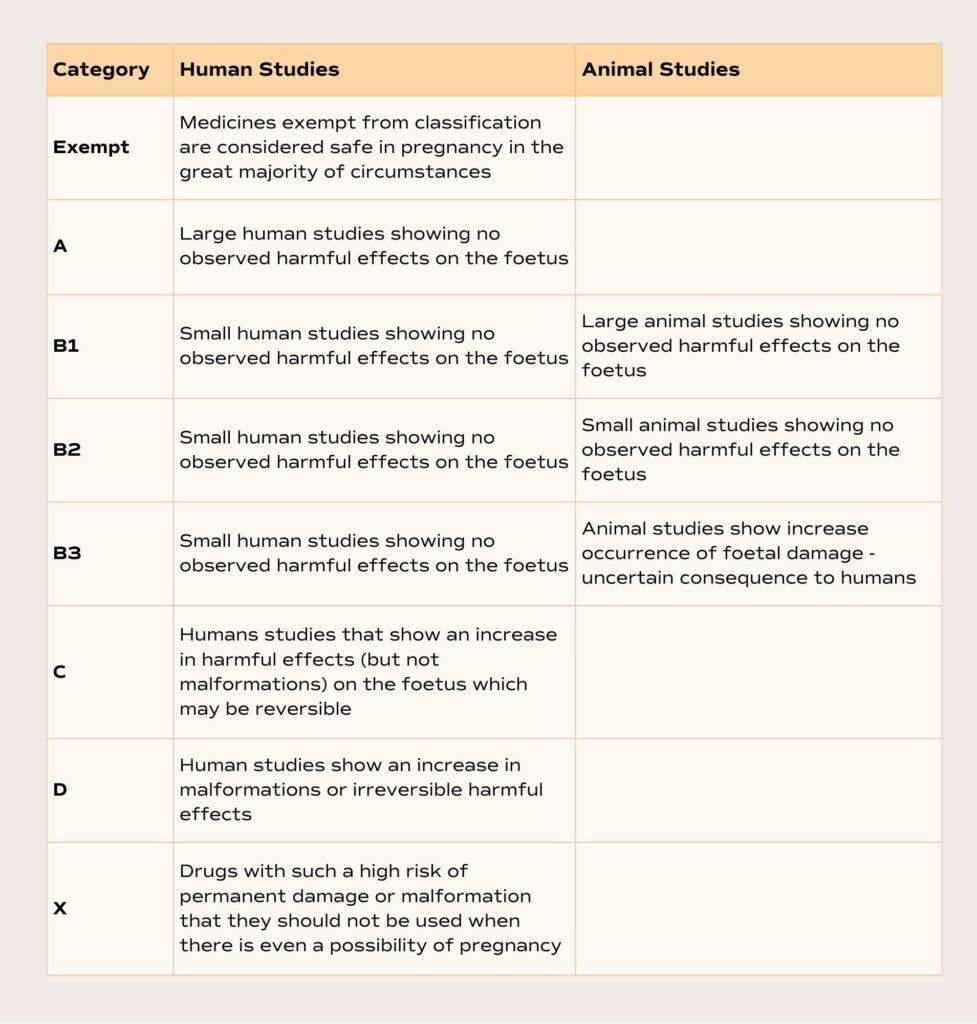
Australian Pregnancy Categories
If safety is important for the general population, then it is ultra important when you’re pregnant. Every mother wants the best for their baby and so to help inform you, the Therapeutic Goods Administration (TGA) have asked medical and scientific experts to assess every medicine for sale in Australia and give each medicine a safety category. This category system is not organised strictly in order of safety, but is arranged by the level of evidence of risk of harm (3).
Natural medicines
- Ginger (eg Morning Wellness PLUS)
Pregnancy Category – Exempt
Treats: Nausea, Vomiting, Dry Retching
Ginger has long been used to treat all kinds of nausea. It is no wonder scientists have looked at it for NVP. In a 2001 study, T Vutyavanich and colleagues found that 87.5% of pregnant women who took 1-2g of ginger each day showed improvement in relieving the severity of their NVP symptoms (1).
The advantage of ginger is that it is abundant, natural, and has a strong unique taste. The downside is that it has a strong unique taste!
1-2g a day of ginger is actually a reasonably substantial dose and difficult to swallow at the best of times – let alone with NVP. It’s best to take it in a form with the minimum impact to your stomach – dissolved in liquid can be effective. Do check your Ginger to make sure you’re getting an effective dose.
Ginger has a slight increase in bleeding tendency, which has also been studied in pregnant ladies. Lindblad and Kopppula (2) found there was a small increase in the frequency of vaginal spotting after 17 weeks (from 5.8% of mums to 7.8% of mums) but no major adverse effects.
Over the Counter Medicines
PUQE Score 4+
If the non-medicines and natural therapies have not helped reduce nausea and vomiting after 1 week, then the next step is to take Vitamin B6.
- Vitamin B6 (eg Morning Wellness)
Pregnancy Category – Exempt
Treats: Nausea, Vomiting, Dry Retching
Vitamin B6 is a nutrient which is essential for human life. We cannot make it in our bodies – we require it in our diet or else more than 100 bodily reactions will cease to happen and we’d be very sick very soon.
Vitamin B6 was first studied in the treatment of NVP in 1942 (4) and has been used and recommended now for over 80 years because it is relatively effective and safe. Not quite a unicorn medicine, but amongst the best of the NVP bunch.
Studies show that on average, taking Vitamin B6 for 7 days will reduce PUQE scores by 56%, and almost half of all ladies will completely stop vomiting within 3 days (13). If you’ve ever had vomiting during pregnancy then it would be a no brainer to try Vitamin B6 for a 50/50 chance of stopping vomiting altogether.
There is almost no upper limit of how much Vitamin B6 we can have each day, but in very high quantities (1000 mg+ per day), for a very long time (months) one might start to get pins and needles, indigestion, breast tenderness or sensitivity to sunlight, which will go away as soon as we stop taking the crazy high dose. For reference the recommended dose of Vitamin B6 for NVP is <100mg/day.
- Antacids
Pregnancy Category – Exempt
Treats: Reflux
In NVP, your stomach can get the gastric equivalent of baby-brain. It forgets how to work – it goes fast, it goes slow, and in HG it can just give up altogether. This is called dysmotility, and it can lead to excess acid in your stomach. When this properly-strong acid finds its way up your throat it’s called reflux – and it burns!
The first step in treating reflux is via antacids. Antacids are a usually minerals – calcium, magnesium or aluminium – in a form for which their pH is very basic (opposite to acid). Hence the name: “anti-acids.” They neutralise some of the acid and this can help settle your tummy if things aren’t too bad to start with.
Be warned, if you over do it with antacids, they can lead to constipation or diarrhoea. Antacids are definitely worth having in your arsenal but often they need a bit of extra help with the prescription reflux treatments in NVP.
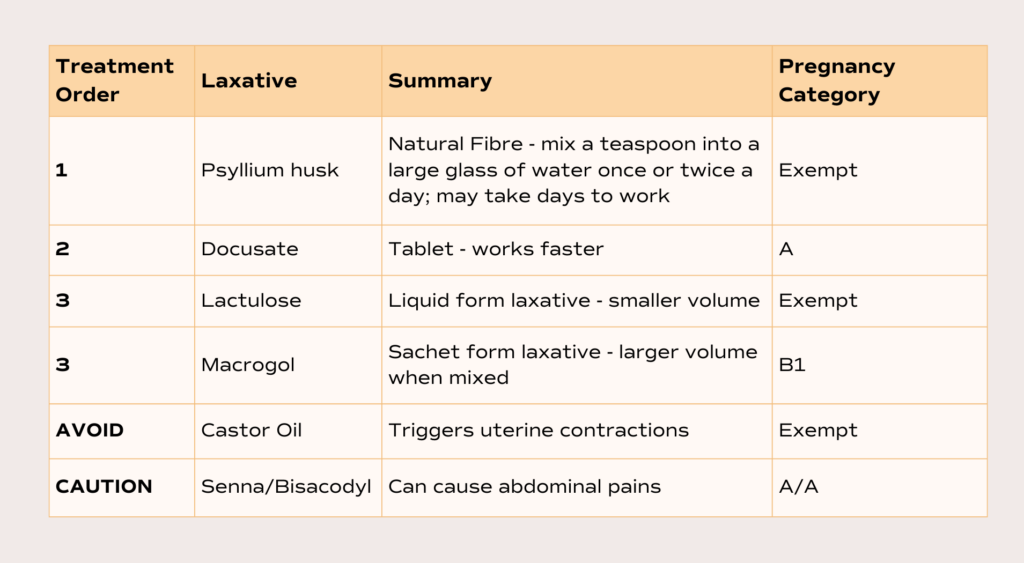
- Laxatives
Pregnancy Category – See table
Treats: Constipation
Similarly to reflux, the dysmotility in your gut caused by NVP can cause constipation. The backlog of output then leads to a different kind of nausea and vomiting. It’s a vicious cycle – it’s particularly important to keep the pipes moving.
The basic elements of a soft stool are water and fibre – give yourself as much of both as you can muster. A blended whole kiwifruit smoothie is a great way to get natural fibre in a tasty way (if you dig kiwi!). Generally the laxative ladder below should get some results, but if not, or if you need them longer than a few days, then it’s time to see the doc.
Pharmacy Only Medicine
PUQE Score 5+
If Vitamin B6 is ineffective alone for decreasing vomiting and nausea, then it is recommended (eTG) to continue to take Vitamin B6 and add doxylamine.
- Doxylamine (eg Restavit)
Pregnancy Category – A
Treats: Nausea, Vomiting, Dry Retching, Insomnia
Doxylamine is a well studied antihistamine. It is not dissimilar to your garden variety hay fever tablet, however in order to stop nausea and vomiting this antihistamine has to cross the blood-brain barrier in order to block the histamine receptors in the vomiting centre of your brain. The catch is, that when an antihistamine is floating around your brain, it causes significant drowsiness and sedation. Caution therefore needs to be used when taking doxylamine and is usually limited to night time, though this can be great for sleep!
Studies show that when combined with Vitamin B6, and taken for 15 days, doxylamine reduced the symptoms of NVP by more than 50% (5).
More common side effects of doxylamine, in addition to the significant drowsiness include dizziness, weakness, headache and lassitude. Less common side effects include palpitations, constipation and reflux (6).
Whilst doxylamine is technically available without a prescription, some pharmacists still prefer a prescription in the context of pregnancy, so if you’re at this rung of the ladder, it might be time to see your doctor.
Prescription Only Medicine
PUQE Score 7+
If Vitamin B6 and doxylamine together are ineffective, then it is recommended to continue to take both Vitamin B6 and doxylamine and speak to a doctor about adding prescription medicines.
Each of the below prescription medicines have a relatively long list of side effects, interactions with other medicines and some have non-negotiable reasons to avoid them. Included are some key side effects for each that you can discuss with your doctor, but (aside from the script) it is integral to consult your doctor to make sure these medicines are right for your circumstance.
- Metoclopramide (eg Maxolon)
Pregnancy Category – A
Treats: Nausea, Vomiting, Dry Retching
Metoclopramide is a common, well studied medication for non-pregnant anti-nausea, however studies for effectiveness in NVP are surprisingly sparse. Metoclopramide increases the speed of your gastro-intestinal tract, which may help settle NVP but it is not necessarily a magic bullet. Some studies show it is comparable to ondansetron in certain circumstances.
It is the lowest risk of harmful outcomes for your baby of the prescription group so the risk of trialling it is lower. Caution must be taken to not take metoclopramide for more than 5 days, and it’s not for mamas under the age of 20. This is to minimise the risk of the more serious and rare ‘extrapyramidal’ side effects.
- Ondansetron (eg Zofran)
Pregnancy Category – B1
Treats: Nausea, Vomiting, Dry Retching
Ondansetron was developed for chemotherapy and in 1991 was considered a major breakthrough in the fight against nausea due to its effectiveness. It has a pregnancy category of B1 because large scale studies on pregnant women have not been completed. It must be noted that there is conflicting data about increased rates of cleft lip and heart malformations in babies of mothers who have taken ondansetron. The frequency of these negative outcomes is so rare it’s difficult to know if it is the normal baseline, or an effect of the medication. Either way, it is something of the order of ~2 affected babies per 100,000 births.
Very common side effects of ondansetron are constipation, headaches and a dry mouth (6). So common is the constipation that most doctors recommend starting laxatives the same day you start ondansetron as there have been cases of complete bowel obstruction due to ondansetron and that’s not pretty.
- Prochlorperazine (Eg Stemetil)
Pregnancy Category – C
Treats: Nausea, Vomiting, Dry Retching
Usually most effective for nausea associated with migraine, vertigo or travel sickness. Given its pregnancy category, it is not usually considered for NVP unless ondansetron or metoclopramide are ineffective but does work well for some mamas.
Prochlorperazine commonly causes constipation, dry mouth, blurred vision or tremor (6).
- Promethazine (Eg Phenergan)
Pregnancy Category – C
Treats: Nausea, Vomiting, Dry Retching
Promethazine is an antihistamine, similar to doxylamine. Whilst they have similar mechanisms of action, and effectiveness, promethazine has increased negative outcomes for the infant. Specifically, when it has been given in high doses during late pregnancy, promethazine has caused prolonged neurological disturbances in the infant. Better to reserve this for specialist care or when options are limited.
- Prednisone
Pregnancy Category – A
Treats: Nausea, Vomiting, Dry Retching
Prednisone is a steroid that does some amazing things. It is very similar to cortisone, our in-built stress hormone and – simulating a stress response – it can dramatically modify our immune system. Virtually every cell in the body has steroid receptors, so its effects are wide ranging – auto-immune suppression, migraine control, nausea reduction, anti-cancer effects, transplant anti-rejection, helps with heart failure and the list goes on.
In short spells, steroids can be wonderful for NVP, however there is possibly a small increased risk of cleft palate when used prior to 10 weeks gestation.
The trouble comes when steroids are used for more than a handful of days: potential Cushing’s syndrome, mood disturbance, high blood pressure, high blood sugar, early breaking of the waters and premature delivery.
It’s good to have steroids on the team, but they need to be used wisely. And FYI, if your doctor prescribes you steroids, you need to increase your Folate to 5mg.
- Famotidine
Pregnancy Category – B1
Treats: Reflux
Famotidine is an antihistamine, however, unlike doxylamine, which works on H1- histamine receptors, famotidine works on H2-histamine receptors. H1-histamine receptors occur mainly on allergy pathways, whilst H2-histamine receptors have more impact in your gastrointestinal tract. The end effect is reduced acid production, and less reflux burning! Famotidine has been used for a long time to help pregnant mamas with reflux so it is a solid option, though there is some suggestion it may increase asthma in babies – discussed further in the Proton Pump Inhibitor section below.
- Proton Pump Inhibitors
Pregnancy Category – Rabeprazole B1; All others B3
Treats: Reflux
Proton pump inhibitors (PPI’s) are almost magical medicines. They block the cellular pump that makes acid in your stomach wall – but only when the acid level is too high. It’s like they know that we still need some acidity but, like perfect Christmas crackling, they never over do it.
There is some suggestion that the use of acid suppression therapy may increase rates of asthma in babies, but the data is unclear exactly when (how many weeks), which (medicines), where (which subgroups of mothers) or why it might be a thing. The best bet is to balance the potential benefits against the potential harms and chat with your doc. This asthma risk applies to all acid suppression therapy, including famotidine (above).
- Mirtazapine (Eg Avanza)
Pregnancy Category – B3
Treats: Depression, Anxiety, Insomnia, Nausea, Vomiting, Dry Retching
Not specifically an anti nausea medication, mirtazapine does have some effects similar to ondansetron for anti-nausea. In addition to this, mirtazapine has anti-anxiety benefits and helps with sleep, so your doctor may suggest this depending on your circumstance.
Hospital Therapies – Outpatient / Day Stay
PUQE Score 13+
If you are in the unlucky minority who have still not been able to get relief from any of the above treatments, or you are so sick you can’t even keep a tablet down, then it might be time to head to the hospital. This is called Hyperemesis Gravidarum and it is a significant disease. You need lots of TLC from your village.
Some hospitals may have a streamlined process to help you avoid the Emergency Department – look up the number for the maternity ward and they’ll point you in the right direction. If in doubt you can always go to the Emergency Department and they will get you the care you need.
Almost certainly you will have an intravenous cannula placed into a vein and a bag of electrolytes started to rehydrate your depleted fluids. IV fluids will make you feel better immediately, so don’t sit at home suffering when wonderful treatment is moments away in hospital.
On top of IV fluids, doctors can offer intravenous anti nausea medication to help keep to NVP away for a while:
- IV ondansetron
- IV metoclopramide
- IV prochlorperazine
- IV hydrocortisone
Hospital Therapies – Inpatient / Hospitalisation
PUQE score 15
At the very pointy end of the sharp stick that is NVP are those mamas who haven’t eaten for so long that the lack of food starts to become a problem. In this circumstance, you’ll probably get a free stay at the local nurse and doctor hotel plus score room service direct to your veins.
In addition to IV fluids and IV medicines, doctors may place a special feeding line called a central line into a large vein. Through this line they will first replace any missing essential vitamins starting with Vitamin B1 (Thiamine) and then step two is to replace all of your nutritional needs via a tube for as long as required. At this level of sickness, the health of the baby is a consideration, so it is very important to have specialist medical care and to not delay reaching out. If you can’t remember your last meal because you’ve been vomiting for so long, then it’s time to pick up the phone or jump in the car.
In the extreme, doctors may consider droperidol, which causes severe sedation, and is a last ditch effort to get mum and bub through to delivery.
In the extreme of the extreme, the mothers life may be at risk due to the severity of symptoms and typically only in these circumstances is a termination considered. Even at this point, the foetus is usually not at risk – an early testament to how mothers prioritise their children’s health over their own health.
Conclusion
Nausea and vomiting during pregnancy is a complex disease with a full spectrum of severity. The best approach is to systematically climb the NVP treatment ladder rung by rung to ensure maximum relief whilst minimising unnecessary side effects.
References
- Vutyavanich, T et al. “Ginger for nausea and vomiting in pregnancy: randomized, double-masked, placebo-controlled trial.” Obstetrics and gynecology vol. 97,4 (2001): 577-82. doi:10.1016/s0029-7844(00)01228-x
- Lindblad, Adrienne J, and Sudha Koppula. “Ginger for nausea and vomiting of pregnancy.” Canadian family physician Medecin de famille canadien vol. 62,2 (2016): 145.
- https://www.tga.gov.au/products/medicines/find-information-about-medicine/prescribing-medicines-pregnancy-database#the-australian-categorisation-system-for-prescribing-medicines-in-pregnancy
- Willis RS, Morris AT, Newsom AA. Clinical observations in treatment of nausea and vomiting in pregnancy with vitamin B1 and B6. A preliminary report. Am J Obstet Gynecol 1942;44:265–71.
- Koren G, Clark S, Hankins GD, Caritis SN, Miodovnik M, Umans JG, et al. Effectiveness of delayed-release doxylamine and pyridoxine for nausea and vomiting of pregnancy: a randomized placebo controlled trial. Am J Obstet Gynecol 2010;203:571.e1–7. http://dx.doi.org/10.1016/ j.ajog.2010.07.030
- https://www.nps.org.au/
- Ghahiri AA, Abdi F, Mastoo R, Ghasemi M. The effect of ondansetron and metoclopramide in nausea and vomiting of pregnancy. JIMS 2011;29:259–65.
- GUIDELINE FOR THE MANAGEMENT OF NAUSEA AND VOMITING IN PREGNANCY AND HYPEREMESIS GRAVIDARUM – Society of Obstetric Medicine of Australia and New Zealand.
- NSW Health Guideline – Nausea and Vomiting in Pregnancy and Hyperemesis Gravidarum https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/GL2022_009.pdf
- https://www.tg.org.au/ Australian Therapeutic guidelines
- Ebrahimi N, Maltepe C, Bournissen FG et al. Nausea and vomiting of pregnancy: using the 24- hour Pregnancy-Unique Quantification of Emesis (PUQE-24) scale. JOGC. 2009;31(9):803-7.
- Furyk JS, Meek RA, Egerton-Warburton D. Drugs for the treatment of nausea and vomiting in adults in the emergency department setting. Cochrane Database of Systematic Reviews. 2015(9):CD010106.
- Babaei, Amir Hossein, and Mahboube Haji Foghaha. “A randomized comparison of vitamin B6 and dimenhydrinate in the treatment of nausea and vomiting in early pregnancy.” Iranian journal of nursing and midwifery research vol. 19,2 (2014): 199-202.